Blunt abdominal trauma can result in clinically significant visceral organ injuries of which the spleen is most commonly affected. Traditional management options for splenic trauma include observation, splenectomy, and splenic artery embolization (SAE). Nonoperative management is preferred for hemodynamically stable patients while splenectomy may be indicated in hemodynamically unstable patients.[1-4] SAE is an alternative nonoperative modality. SAE can be performed proximally or distally, with proximal SAE offering lower rates of splenic infarction and shorter procedure times but complicating future coaxial interventions, while distal SAE improves splenic salvage in cases of focal injury but increases infarction risk.[2-5]
In liver transplant patients, managing splenic injury can be more complex due to altered vascular anatomy. Splenic artery steal syndrome (SASS) is a rare but severe complication seen after liver transplantation where shunting of blood from the hepatic artery to the splenic artery leads to hepatic hypoperfusion and potential graft dysfunction. Splenic artery ligation is sometimes performed prophylactically to prevent SASS, but this can complicate future interventions, as seen in this case.[6,7]
This case report describes emergent splenic embolization through gastroepiploic artery (GEA) in a liver transplant recipient with previous splenic artery ligation following acute trauma.
CASE REPORTA 30-year-old male with history of an orthotopic liver transplant and a combined kidney and second liver transplant presented to the emergency department following a motorcycle accident. On initial assessment, he was alert and oriented, complaining of right shoulder and left chest pain. His blood pressure (BP) dropped to 84/47 mmHg, and heart rate (HR) rose to 114 beat/min.
A focused assessment with sonography in trauma (FAST) scan revealed free fluid. After receiving blood products, BP stabilized at 123/83 mmHg, although HR remained between 110 and 119 beat/min. He was taken for computed tomography (CT) scan which demonstrated a Grade 5 splenic laceration with hemoperitoneum [Figure 1], multiple left rib fractures, and left scapular fractures. Despite previous splenic artery ligation, the entire artery was patent, evidenced by contrast opacification. In addition, a largely hypertrophied GEA was noted [Figure 2]. Interventional radiology was consulted for emergent embolization.
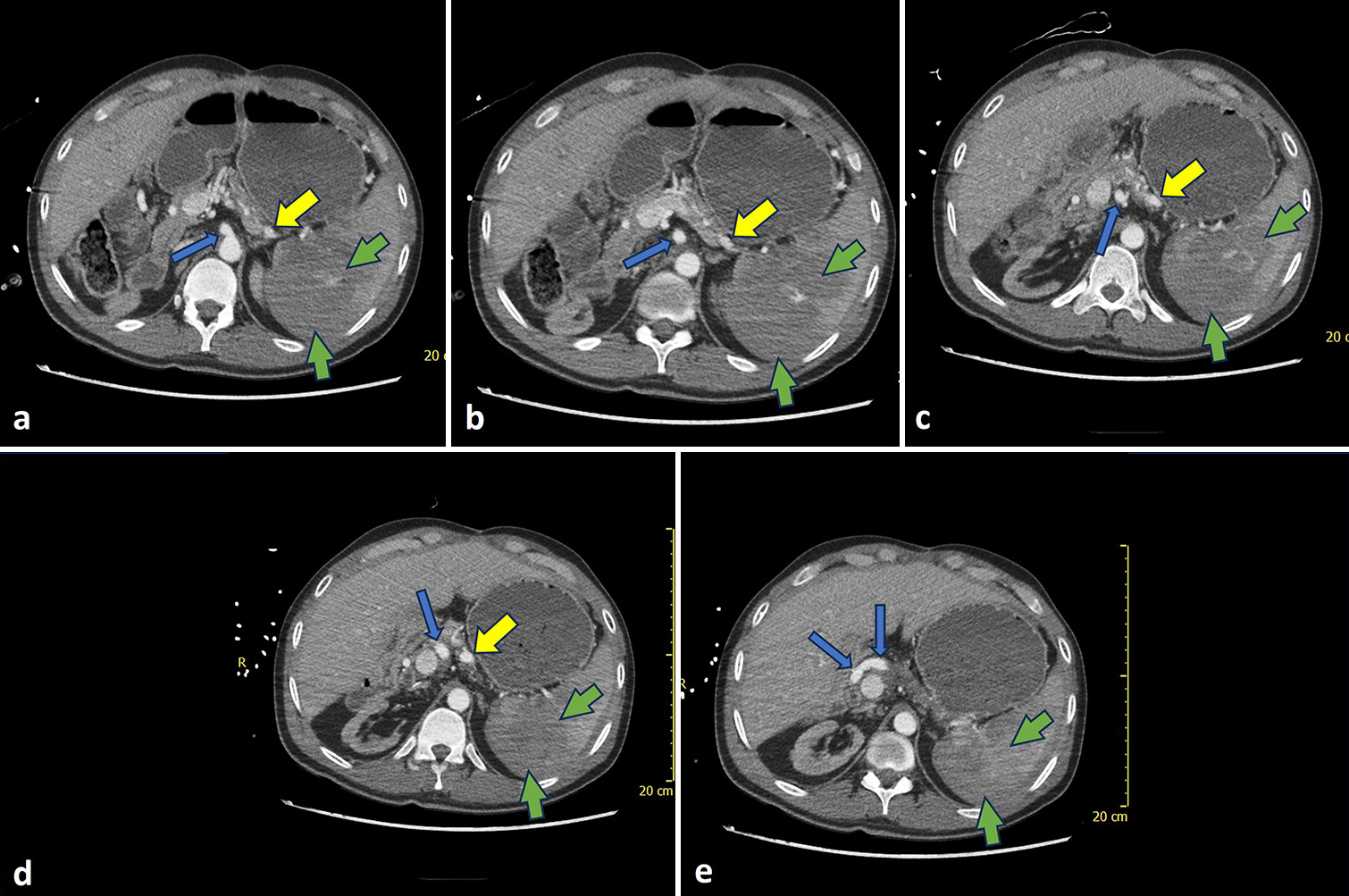
Export to PPT
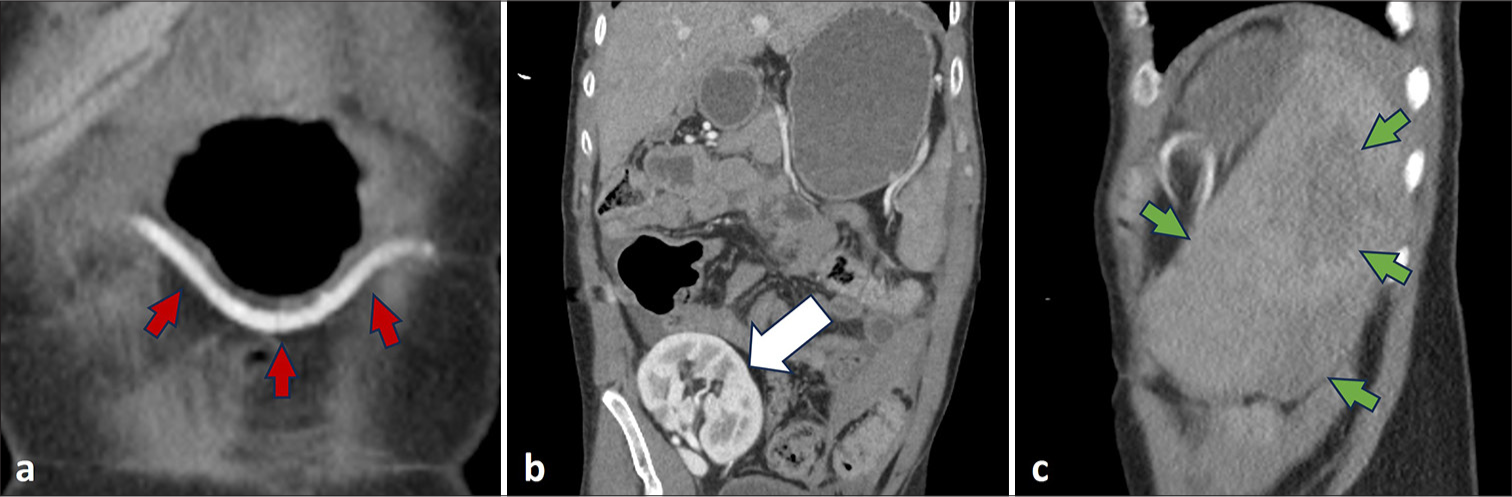
Export to PPT
The celiac trunk was accessed using a 65 cm 5F SOS catheter (AngioDynamics, Latham, New York) through a right femoral artery puncture. Arteriography demonstrated a dilated and tortuous gastroepiploic artery (GEA) originating as usual from common hepatic and gastroduodenal arterial segments. Without an inner wire, the catheter was gently retracted and twisted so that its loop was less acutely angulated. Simultaneously, its tip was advanced into a common hepatic branch near the origin of the gastroduodenal artery (GDA). A stiff angled glide wire (Terumo, Somerset, New Jersey) was advanced through the GDA, right and subsequently left GEA segments. The SOS catheter was readily advanced over the wire and then exchanged for a more simple angle tipped 100 cm 5F hydrophilic catheter. The stiff angled glide wire was replaced with a non-stiff glide wire.
The left GEA was markedly redundant and tortuous, especially near the splenic hilus [Figure 3]. Distal embolization close to the splenic hilus was preferred to avoid embolization of gastric and pancreatic segments arising proximally from the GEA. The 100 cm catheter could not reach close enough to the splenic hilus; therefore, the glide wire was removed and a 130 cm 2.8F Progreat microcatheter (Terumo, Somerset, New Jersey) assembly was advanced through the 5F catheter until maximal length of the inner coaxial system achieved satisfactory proximity to the splenic hilus. Angiography demonstrated extravasation. The microwire was removed and a gelatin foam slurry including diluted contrast was injected for embolization. Post-embolization arteriography confirmed successful pruning and no extravasation [Figure 4]. The coaxial apparatus was removed, and hemostasis was achieved through manual compression.
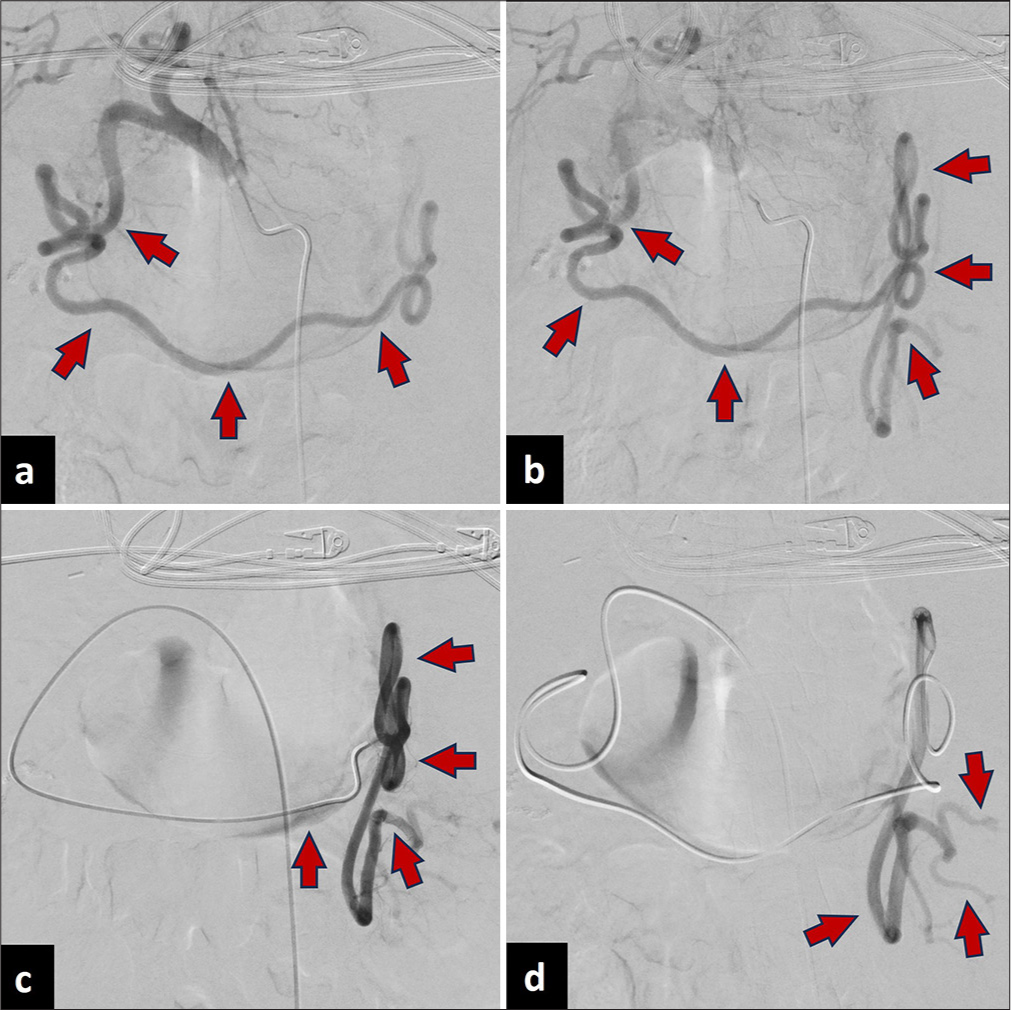
Export to PPT
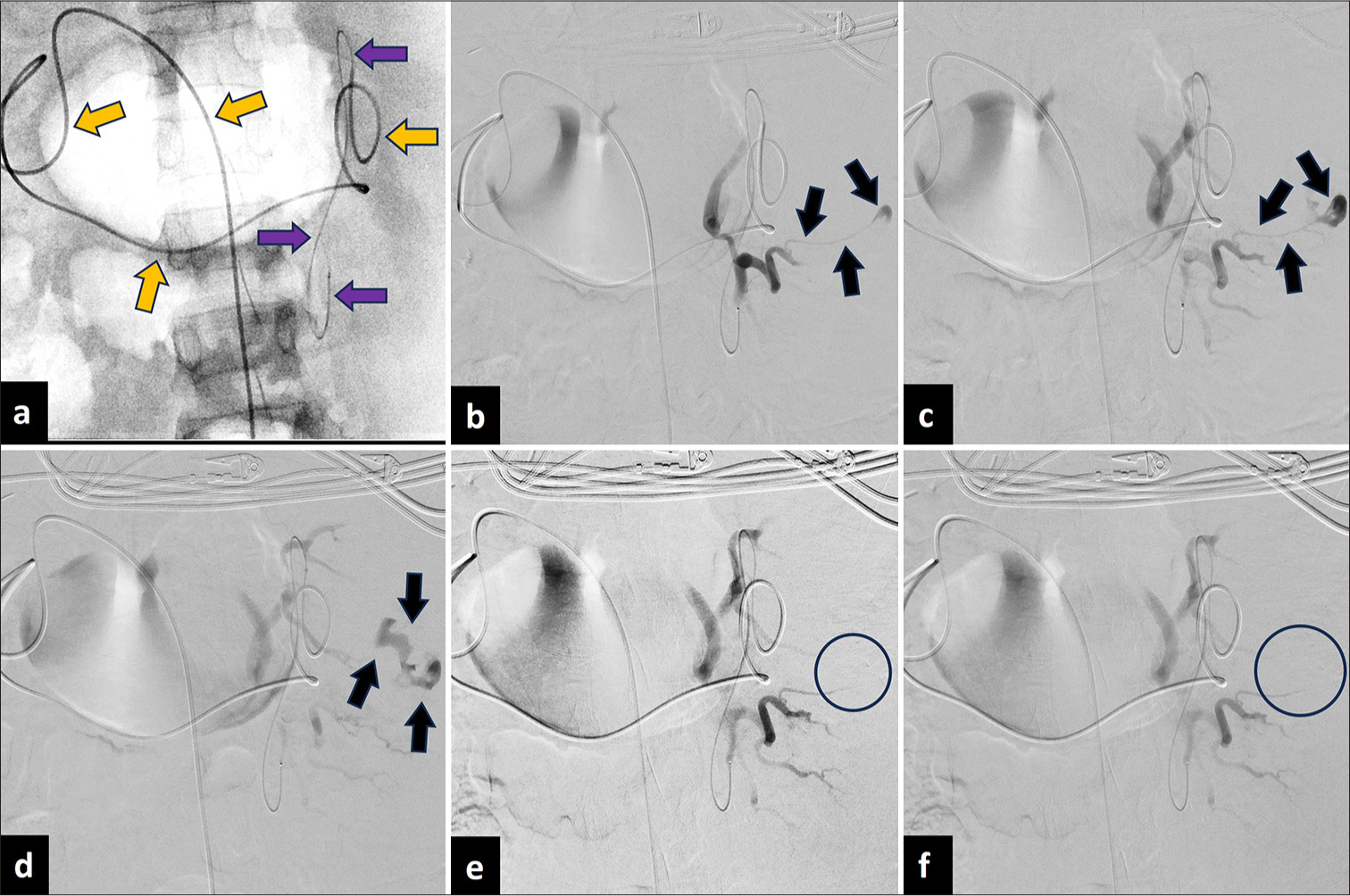
Export to PPT
The patient’s BP was 134/88 mmHg, and HR was 109 bpm during manual compression. He was transferred to the surgical intensive care unit (ICU) and later to a non-ICU bed before being discharged to his transplant center a week later.
DISCUSSIONInitial radiologic examination for blunt splenic trauma is a focused assessment with sonography in trauma (FAST) examination. Following a positive FAST, computed tomography (CT) with intravenous contrast is indicated. The American Academy of Surgery and Trauma splenic injury scale is used to grade the degree of splenic injury from I to V, with a high-grade injury characterized as greater than Grade III.[1-4] Hemodynamically stable patients with any grade of splenic injury are candidates for SAE. The goal of SAE is to reduce a high flow arterial flow to the site of injury. Proximal embolization achieves this by occluding the main splenic artery, whereas distal embolization selectively targets branch vessels.[4] Embolization can be performed using vascular plugs, coils/microcoils, gelatin foam, particles, or glue.[2-5]
SAE typically involves femoral artery puncture, celiac trunk selection, and splenic artery catheterization. However, in this case, given the prior splenic artery ligation, conventional embolization through the splenic artery was not feasible. Alternative approaches, such as surgical splenectomy or embolization through collateral pathways, were considered. However, splenectomy was avoided due to the risks of overwhelming post-splenectomy infection, particularly in an immunosuppressed transplant patient. The hypertrophied GEA was identified as a viable access route, providing a direct path to the spleen while preserving hepatic perfusion. This approach was deemed the safest and most effective method to control hemorrhage while minimizing potential complications.
Bashir et al. reported a case in which partial SAE was performed through right GEA in a patient post-liver transplantation with prophylactic splenic artery ligation. There were no reported complications immediately post-procedure and at 5 months follow-up.[8] Xu et al. reported a similar case in which partial SAE was performed following selections of GEA and dorsal pancreatic arteries in a patient post splenic artery ligation but without liver transplantation. Reported post-procedure complications included moderate fever and left upper abdominal pain which lasted for 15 days.[9] In both reports, embolization was performed using polyvinyl alcohol particles and the intervention was performed for the treatment of hypersplenism. Unlike these prior cases, our case involved emergent embolization with a gelatin foam slurry due to trauma rather than elective intervention for hypersplenism. In addition, no similar post-procedural complications in addition to gastric ischemia or pancreatic infarction were observed, reinforcing the feasibility of this approach in emergency settings. Loss to follow-up after the patient was transferred to his transplant facility was a limitation. In the case of acute trauma, it is important to review relevant anatomy on prior imaging to accurately perform a well-informed swift intervention.
CONCLUSIONThis case describes emergent splenic embolization through a hypertrophied and tortuous GEA following blunt abdominal trauma in a liver transplant recipient with prior splenic artery ligation. By demonstrating the viability of this alternative embolization route, this case provides insight into managing complex vascular anatomy in trauma settings. When routine procedures are complicated by altered vascular anatomy, careful imaging review is essential to guide successful intervention.
Comments (0)