Dear Editor,
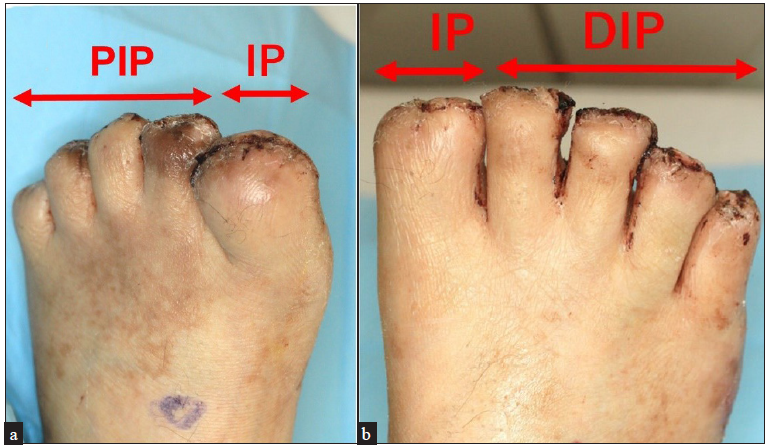
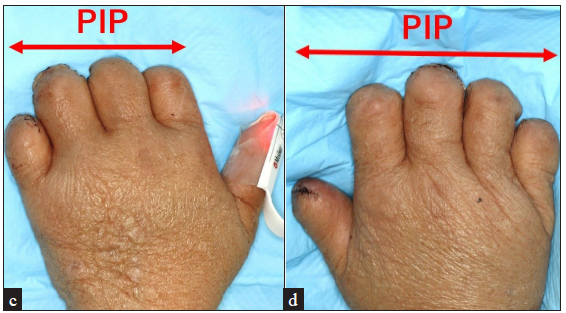
A 72-year-old man presented to the emergency department with a 5-day history of a slight fever and haematochezia. The patient had a past medical history of acquired haemophilia A and hepatocellular carcinoma. On physical examination, he was febrile and in shock (temperature 38.5 degrees, heart rate 110 bpm, systolic blood pressure 50 mmHg). Gastrointestinal endoscopy and a contrast-CT of the abdomen and pelvis were performed but they failed to identify the source of the bleeding or infection. During the endoscopy, he developed aspiration pneumonia and was intubated and admitted to the medical intensive care unit (ICU). He was treated for sepsis empirically with piperacillin–tazobactam. Initial blood examination showed a white blood cell count of 2.4 × 103/μL, red blood cell count of 351 × 104/μL, platelet count of 4.7 × 104/μL, CRP of 15.81 mg/dL, lactate of 5.72 mmol/L, PT INR of 2.4 and fibrinogen of 154 mg/dL. He was given fluid resuscitation, intravenous norepinephrine and vasopressin and a blood transfusion. Continuous veno-venous haemodialysis was necessary by the eighth day of admission due to acute renal failure. Blood cultures and a urine culture both grew Streptococcus dysgalactiae subspecies equisimilis (SDSE). It was noticed that his left shoulder was swollen within the first few days of admission and a shoulder joint aspirate fluid culture also grew SDSE. Piperacillin–tazobactam was substituted with penicillin G and clindamycin. On the sixth day of admission, he developed skin necrosis on the tips of all the fingers and toes [Figures 1a–1d]. Serum protein C activity was 41% (normal range, 64–146%) and protein S activity was 71% (normal range, 67–164%). A biopsy was attempted from the digits; however, a satisfactory sample could not be obtained due to the degree of necrosis. His general condition gradually improved with the treatment and he had his fingers and toes amputated 2 months after admission [Figures 2a–2d and 2e–2h].

Export to PPT
Export to PPT
Export to PPT

Export to PPT
Given the clinical presentation over the extremities accompanied by a history of septic shock and evidence of acute clotting disturbance, a diagnosis of symmetrical peripheral gangrene (SPG) was made.
SPG is a life-threatening condition characterised by a triad of shock, disseminated intravascular coagulation (DIC) and anticoagulant depletion.1 It has been speculated that a reduction in protein C is involved in the aetiopathogenesis.1 SPG is associated with a high mortality and it has been reported that more than half of the surviving patients required amputations of the limbs.2,3 In the present case, fortunately, the necrotic area was localised and amputation at the level of interphalangeal joints was adequate.
Many causes for SPG have been identified. Non-infectious causes include acute or chronic liver disease and iatrogenic causes including vasopressor use and colloidal transfusions.1,2 Various infective agents have been reported to be associated with SPG, including common agents such as Pneumococci, and E. coli and rare agents such as Serratia marcescens and SARS-CoV-2.3–6 The exact incidence of these causative factors cannot be determined due to the rarity of SPG, but it has been suggested that pneumococcal sepsis is the most common infectious cause of SPG with one study reporting its association with 28.5% of cases.4 In the same study, E. coli was found to be associated with 14.3% of cases.4 Our patient had SDSE infection which has not been reported to be associated with SPG previously. SDSE is a group C or G β-hemolytic streptococci that resides in the human nasopharynx, skin and perineum. Several clinical case series have reported SDSE infections to be more common among elder adults and in individuals with underlying chronic illnesses. SDSE has been implicated in a wide variety of human infections and the incidence of invasive disease due to SDSE may be increasing.7 Because of these characteristics, we envisage SDSE infections to become a significant health burden in the near future, given the ageing population in developed countries. The present case highlights the importance of rapid identification of SDSE, as it has the potential to cause extremely serious complications with high mortality like SPG.
Comments (0)