Many individuals suffer from skin conditions for several years, even a lifetime. Such conditions are often immediately visible to others and patients feel self-conscious. Many go through mental distress such as depression, anxiety and poor self-esteem which need to be managed. This study administered mindful self-compassion training in adults with skin conditions who reported high levels of depression, anxiety and stress. Participants were requested to fill questionnaires before and after the intervention was provided. The group of participants who received the intervention for 4 weeks were compared to another group of participants who did not receive the intervention, and the pre-test and post-test scores were compared. Results indicated that the group of participants who received the intervention had reduced levels of depression, anxiety and stress as compared to the control group who did not receive the intervention. They also had improved levels of self-esteem, well-being and quality of life. Such an intervention can be effectively used to manage psychological distress in individuals with skin conditions. Mental health professionals and dermatologists together can provide patients with holistic treatment. In view of ethical equality, the control group was also provided with mindful self-compassion training after the end of the study.
IntroductionRecent research on the burden of chronic skin diseases and associated distress has shown psychological, social and financial costs on patients and families.1 Patients with chronic skin conditions often go through multiple hurdles, which impairs their psychosocial functioning.2 Many studies worldwide indicate associated mental distress in skin conditions. Research has found association of dermatological conditions with clinical depression,3-8 clinical anxiety,5,6 suicidal ideation,3,4,9 low self-esteem10–12 and poor quality of life.6,10,12 Skin diseases are different from internal illnesses since they are often immediately noticeable to others. One’s appearance may differ from the normal. The visibility of such conditions make them ‘life-ruining’, and persons with disfigurement often feel devastated.13 Individuals face stigma due to this apparent nature of skin conditions and develop a constant fear of stigma, which impacts their lives negatively.2,8 Many go through problems of teasing, taunting and bullying.14 They experience poor social functioning,6,7,9 decreased interactions,9,11 loneliness7 and social phobia.13
The benefits of mindfulness interventions for mental and physical health outcomes have been established by research.15 Meta-analytic and systematic review studies indicate that mindfulness-based interventions show improvement in depression,16,17 anxiety17,18 and stress.17,19 Such interventions decrease emotional distress in psoriasis,20,21 acne21 and eczema.21,22 Self-compassion interventions have shown significant improvement in rumination, stress, depression, self-criticism and anxiety.23 Patients with chronic skin conditions go through a lifelong struggle. However, the psychosocial part of management remains overlooked.7 Mindful self-compassion can cover this treatment gap. It is a resource-building mindfulness-based self-compassion training programme that uses a combination of personal development, training and psychotherapy designed to enhance one’s capacity for self-compassion by cultivating spacious awareness as a basis for compassionate action.24,25
Hence, we conducted a study to assess the impact of this intervention on depression, anxiety, stress, dermatology-specific quality of life, self-esteem and well-being in adults suffering from chronic skin conditions.
MethodsThe research was conducted after approval by the ethical committee of Amity Institute of Behavioural and Allied Sciences, Amity University, Mumbai (Letter No. AUM/AIBAS/EC/2022/01). Purposive sampling technique was used. Participants were recruited from two private dermatology skin clinics in Mumbai, after debriefing dermatologists and taking permissions. The two clinics were Sparsh clinic and Gosavi’s skin clinic. These patients were visiting dermatologists for their skin concerns and were receiving concurrent pharmacological care. Initially 422 participants aged 18–55 years with heterogeneous skin conditions completed forms giving their socio-demographic details, clinical characteristics, as well as self-reported Depression, Anxiety and Stress Scale–21 questionnaire (DASS-21), which assesses levels of depression, anxiety and stress. Informed and written consent was taken beforehand.
The inclusion criteria were voluntary participation, having a symptomatic skin condition for a minimum of 6 months, receiving a formal diagnosis from a dermatologist, proficiency in English for completing self-report questionnaires and to engage in the intervention,psychological distress (experiencing higher levels of depression, anxiety and stress based on the scale and scores above cut-off). Exclusion criteria included those receiving any concurrent treatment for a mental illness, those already practising specific mindfulness meditation techniques, those reporting current thoughts or acts of self-harm or suicide and pregnancy. Shortlisted participants were contacted and debriefed about their scores and psychological distress. They were educated about mental health services and treatment options. Those interested in participating in the study were requested to fill the Dermatology Quality of Life Scale, Rosenberg Self-Esteem Scale and World Health Organization Well-Being Index to obtain pretest scores.
A waiting-list control design was used where participants were randomised to the intervention condition or waitlist control group. Messages and emails were sent to the participants with details of the study, dates, timing and Google meet link with reminders. In the first and last sessions, they were told about the concept of mental health and illness, their high distress scores and the need to seek services from psychiatrists and clinical psychologists. The intervention was used in a group format over a period of 4 weeks with online sessions taking place twice a week. Participants could attend either a morning or an evening session based on their convenience. The intervention was conducted by two trained clinical psychologists. Each session lasted 50 minutes. Different guided mindfulness and self-compassion techniques (for example, exercises like providing a soothing touch to self and writing a compassionate letter towards the self) were practised in every session to induce grounding and relaxation and their rationale was explained. The facilitators also elicited discussions to change the approach of participants and develop an approach towards the self with kindness, common humanity, mindfulness, acceptance and gratitude. Participants who completed all eight sessions were requested to fill the questionnaires again as a post-test outcome measure. To maintain ethical guidelines, the waitlist control was provided with the same intervention after data collection.
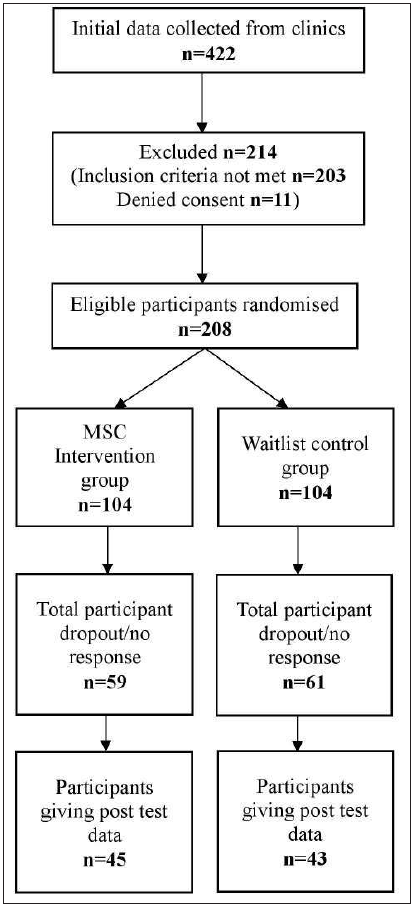
The final sample consisted of 88 participants [Figure 1]. All data analyses were performed using the software Statistical Package for the Social Sciences (SPSS), Version 27.
Export to PPT
ResultsThe demographic distribution and clinical features of the participants has been showcased in Tables 1 and 2, respectively. Acne was the most common disorder, in 29 (32.9%) participants. Thirty-one participants were in the age group of 36–45 years (35.2%). The study comprised 59 females (67%) and 29 males (33%).
Table 3 indicates the mean pre-test and post-test scores for each domain. At the end of the study, the mean scores for depression, anxiety, stress and dermatology life quality index on post-test evaluation were found to be lower for the intervention group as compared to the waitlist control group. The mean scores for well-being and self-esteem on post-test evaluation were found to be higher for the intervention group as compared to the waitlist control group.
ANCOVA was used to test for differences in levels of depression, anxiety, stress, dermatology life quality index, self-esteem and well-being between the intervention and waitlist-control groups. For each domain, the pre-test scores were used as a covariate to assess for post-test differences between the intervention group and waitlist control group. The difference in means of depression, anxiety, stress, dermatology life quality index, self-esteem and well-being between the intervention group and waitlist control group was found to be statistically significant using the ANCOVA model (p < 0.001) [Table 4]. At the end of the study, the intervention group had reduced psychological distress and enhanced dermatology-specific quality of life, self-esteem and well-being as compared to the waitlist control.
Table 1: Demographic distribution of participants
Domain MSC intervention group (n = 45) Waitlist control group (n = 43) Total Age in years 18–25 13 (28.9%) 11 (25.6%) 24 (27.3%) 26–35 14 (31.1%) 11 (25.6%) 25 (28.4%) 36–45 17 (37.8%) 14 (32.6%) 31(35.2%) 46–55 1 (2.2%) 7 (16.3%) 8 (9.1%) Sex Male 14 (31.1%) 15 (34.9%) 29 (33%) Female 31 (68.9%) 28 (65.1%) 59 (67%) Highest educational qualification Senior secondary 8 (17.8%) 10 (23.3%) 18 (20.5%) Graduate 24 (53.3%) 24 (55.8%) 48 (54.5%) Postgraduate 13 (28.9%) 8 (18.6%) 21 (23.9%) Super speciality 0 1 (2.3%) 1 (1.1%) Religion Hindu 26 (57.8%) 31 (72.1%) 57 (64.8%) Muslim 10 (22.2%) 6 (14%) 16 (18.2%) Jain 4 (8.9%) 1 (2.3%) 5 (5.7%) Sikh 2 (4.4%) 3 (7%) 5 (5.7%) Christian 3 (6.7%) 2 (4.7%) 5 (5.7%) Socio-economic Status Upper 14 (31.1%) 12 (27.9%) 26 (29.5%) Middle 31 (68.9%) 31 (72.1%) 62 (70.5%) Low 0 0 0 Marital Status Married 29 (64.4%) 24 (55.8%) 53 (60.2%) Unmarried 16 (35.6%) 19 (44.2%) 35 (39.8%) Employment Status Employed 25 (55.6%) 19 (44.2%) 44 (50%) Unemployed 20 (44.4%) 24 (55.8%) 44 (50%)Table 2: Clinical features distribution
Skin condition MSC intervention group (n = 45) Waitlist control group (n = 43) Total (n = 88) Acne 15 (33.3%) 14 (32.5%) 29 (32.9%) Atopic Dermatitis 11 (24.4%) 10 (23.2%) 21 (23.8%) Psoriasis 6 (13.3%) 6 (13.9%) 12 (13.6%) Vitiligo 4 (8.8%) 4 (9.3%) 8 (9%) Rosacea 3 (6.6%) 3 (6.9%) 6 (6.8%) Other 5 (1.1%) 2 (4.6%) 7 (1.1%) 2 or more 1 (2.2%) 3 (6.9%) 4 (4.5%)Table 3: Comparisons between the intervention and waitlist control groups for pre-test and post-test scores
MSC intervention group Waitlist control group Pre-test (Mean ± SD) Post-test (Mean ± SD) Pre-test (Mean ± SD) Post-test (Mean ± SD) Depression 14.95 ± 2.41 3.20 ± 1.70 15.27 ± 2.23 15.33 ± 2.03 Anxiety 12.66 ± 2.70 2.76 ± 1.88 13.58 ± 2.24 13.81 ± 2.11 Stress 16.31 ± 1.26 4.89 ± 1.78 16.79 ± 1.37 16.44 ± 1.46 Dermatology Quality of Life 23.86 ± 4.67 10.02 ± 3.68 24.76 ± 3.58 24.84 ± 4.04 Self-esteem 15.84 ± 1.53 24.56 ± 0.72 26.11 ± 1.64 26.07 ± 1.59 Well-being 11.86 ± 2.46 22.20 ± 1.63 8.32 ± 2.16 8.33 ± 1.83Table 4: ANCOVA model for tests of between-subjects effects using pre-test scores as covariates
Measurement F Significance Partial ETA squared Depression 1789.554 P < 0.001 0.995 Anxiety 1105.770 P < 0.001 0.929 Stress 1561.326 P < 0.001 0.948 Dermatology quality of life 712.097 P < 0.001 0.893 Self-esteem 43.324 P < 0.001 0.338 Well-being 1160.759 P < 0.001 0.932 DiscussionThe results indicate that mindful self-compassion (MSC) was effective and showed significant reduction in psychological distress in individuals with chronic skin conditions. This is consistent with previous studies where mindfulness and self-compassion based interventions have shown reduction in depression,20,26,27 anxiety20,26,27 and stress,20,22,27 and boosted levels of dermatology-specific quality of life,20,27,28 self-esteem21 and well-being.26,28
Mindfulness fosters awareness of the present moment, which enhances the vividness of life. Individuals with skin conditions face stigma,2,8 fear of stigma,2,8 humiliation,13 teasing,14 taunting,14 bullying,14 social phobia,13 poor socialisation.6,7,9,11 Their attention remains in their disfigurement and they neglect other experiences, self-criticise, ruminate about the past, or worry about the future.15 The awareness, relaxation and acceptance as a result of mindfulness reduced the experiential avoidance, self-judgment and rumination which is associated with depression, anxiety and low self-esteem.15,29 It enhances emotional regulation and helps cope with challenges.29 This protects one from the impact of stress associated with skin diseases and affects stress-related disease outcomes like dermatology-specific quality of life, self-esteem and well-being.29 Self-compassion helped participants become gentle, forgiving, supportive and sympathetic towards themselves. Participants realised that perfection is unrealistic, all humans are flawed and that negative experiences are universal. Disfigurement, bullying, teasing, rejection, criticism, loneliness, stigma are faced by many.24,25
This study indicates how a mindfulness and self-compassion-based intervention is effective for psychological distress associated with skin conditions. It also highlights the need for psycho-dermatology liaison services. Dermatologists should be wary of emotional disturbance in patients and can give referrals to mental health professionals when required. This intervention can be used effectively by mental health professionals and treatment protocols can be created for psycho-dermatology settings.
LimitationsThe current study has certain limitations and scope for future research. The sample consisted of heterogeneous skin conditions. Further mindful self-compassion intervention studies can be done to understand the impact on specific skin conditions. Due to time constraints, we could not employ qualitative methods to assess subjective experiences of participants or gather follow up data to assess long-term effects. We also could not assess reasons for participant dropouts. Lastly, the sample consisted of participants from middle and upper socio-economic class only.
ConclusionMindful self-compassion can be used to manage psychological distress in skin conditions. Dermatologists can become acquainted with basic signs of mental distress and the importance of psychological interventions. By collaborating with mental health professionals, patients can be given holistic treatment.
Comments (0)